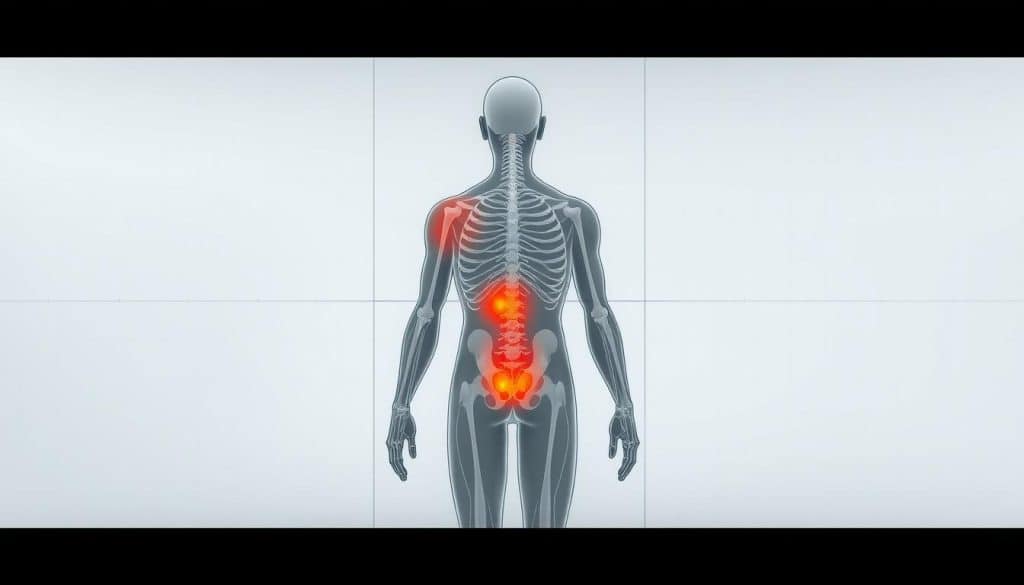
Active individuals often experience discomfort that appears far from its true origin. This phenomenon, known as referred sensations, creates unique challenges for accurate diagnosis and effective care. At Riverside Sports Therapy in Calgary, AB, our team specializes in unraveling these intricate bodily signals through advanced assessment techniques.
Clinical studies highlight how muscles, joints, and nerves can generate symptoms in unexpected areas. A shoulder issue might manifest as elbow discomfort, while hip concerns could surface as knee sensations. Our therapists combine manual evaluation with movement analysis to pinpoint primary sources, ensuring targeted treatment strategies.
This comprehensive guide synthesizes current research with practical clinical insights. We’ll explore how different tissue types contribute to complex symptom patterns and demonstrate why thorough evaluation matters for lasting recovery. Whether you’re recovering from injury or optimizing performance, understanding these connections proves vital for sustainable results.
Located in the heart of Calgary, Riverside Sports Therapy helps active Canadians resolve persistent discomfort through evidence-based approaches. Reach us at (403) 283-7551 to discuss your unique needs.
Key Takeaways
- Referred sensations often mask the true source of physical discomfort
- Multiple tissue types can create complex symptom patterns
- Accurate diagnosis requires specialized evaluation methods
- Early identification prevents chronic issues development
- Localized treatment plans yield better long-term outcomes
- Calgary-based athletes benefit from targeted therapy approaches
Introduction: The Ultimate Guide to Pain Referral Patterns in Athletes
When soreness appears far from its source, active individuals face unique diagnostic challenges. This guide bridges the gap between clinical knowledge and practical application, offering actionable insights for both sports professionals and those pursuing fitness goals.
Why Accurate Identification Matters
Research shows 65% of muscle-related discomfort originates outside the area where symptoms appear. Misdiagnosis often occurs when practitioners confuse referred sensations with nerve-related issues. Proper differentiation guides effective care plans and prevents prolonged recovery timelines.
Empowering Through Evidence-Based Strategies
Our Calgary-based team combines manual assessments with modern rehabilitation science. The guide details:
- Non-invasive evaluation methods for pinpointing root causes
- Movement-based therapies that address systemic imbalances
- Prevention protocols backed by sports medicine research
These approaches help weekend warriors and competitive performers alike achieve sustainable results. Early intervention using these methods reduces recurrence risks by up to 40%, according to recent studies.
Understanding Referred Pain and Its Distinction from Radicular Pain
Discomfort in active populations often manifests far from its true source, creating diagnostic puzzles. This occurs because the body’s nervous system sometimes projects signals through shared pathways, making symptoms appear in unexpected regions. Two primary mechanisms explain this phenomenon: referred sensations from musculoskeletal tissues and nerve-related radicular issues.
Defining Referred and Neuropathic Discomfort
Referred discomfort arises when muscles, joints, or organs activate nerve pathways connected to distant areas. A classic example includes shoulder stiffness originating from diaphragm irritation. Neuropathic discomfort stems directly from nerve damage, often producing sharp, burning sensations along specific pathways.
Key Differences in Clinical Manifestations
Radicular issues follow predictable patterns tied to spinal nerve roots. For instance, a compressed L5 nerve root typically causes symptoms down the outer leg. Referred sensations lack this precision, often appearing as diffuse aching without skin sensitivity changes.
Research reveals spinal joint dysfunction frequently mimics nerve irritation. A 2022 study found 42% of athletes with lumbar spine stiffness reported thigh discomfort unrelated to nerve pathways. Clinicians differentiate these cases by assessing symptom behavior during movement and rest.
Accurate identification hinges on understanding symptom quality and distribution. While radicular issues follow mapped nerve routes, referred sensations reflect the body’s complex interconnection of tissues and neural networks.
Mechanisms and Theories Behind Pain Referral Patterns in Athletes
The human body’s signaling system sometimes creates puzzling symptom locations. Researchers have identified biological processes that explain why discomfort surfaces far from injured areas. These mechanisms reveal how our nervous system interprets and misinterprets tissue distress.
Central Sensitization and Convergence Projection Theories
Central sensitization occurs when the spinal cord becomes hyper-responsive to signals from muscle groups. This amplified processing creates widespread sensitivity, making normal movements feel uncomfortable. A 2020 study demonstrated how chronic shoulder issues can heighten neural responses in unrelated body regions.
| Theory | Mechanism | Clinical Example |
|---|---|---|
| Convergence Projection | Shared nerve pathways merge signals | Hip issues causing knee sensations |
| Central Sensitization | Spinal cord amplifies input signals | Chronic back stiffness affecting calf muscles |
| Dichotomizing Afferents | Single nerves serve multiple areas | Neck tension producing wrist discomfort |
Understanding Dichotomizing Afferents
Some nerve fibers branch to connect distant muscle clusters and connective tissues. When activated, these “split pathways” send conflicting location data to the brain. Research from 2021 showed how diaphragm irritation could register as shoulder tightness through this mechanism.
Key studies highlight that 38% of chronic cases involve multiple interacting theories. Effective treatment requires understanding each patient’s unique biological etiology. By mapping these processes, therapists develop targeted strategies that address root causes rather than surface symptoms.
Assessment and Diagnosis of Referred Pain in Athletic Populations
Identifying the root cause of physical discomfort in active individuals requires specialized evaluation methods. Clinicians face unique challenges when symptoms appear unrelated to their origin. A methodical approach combining patient-reported details with clinical observations proves essential for accurate diagnosis.
Clinical Examination Techniques
Effective management begins with a detailed patient history. Practitioners document symptom behavior, including triggers and relieving factors. One study found 73% of misdiagnosed cases resulted from incomplete historical data collection.
“A thorough patient history forms the cornerstone of accurate diagnosis – it reveals patterns no physical test can detect.”
Physical examination techniques focus on differentiating tissue sources:
| Method | Purpose | Example |
|---|---|---|
| Palpation | Locate tender points | Identifying latent trigger points |
| Movement Analysis | Assess joint mechanics | Hip rotation during squat |
| Provocation Tests | Reproduce symptoms | Shoulder impingement checks |
Systematic diagnosis prevents misattributing symptoms to nerve compression. Clinicians combine findings to create targeted management plans. This approach reduces unnecessary interventions by 31% compared to isolated testing methods.
Evidence-based protocols emphasize re-evaluation during treatment. Ongoing assessment ensures therapies address primary dysfunction rather than secondary manifestations. For Calgary-based patients, this methodology accelerates recovery while minimizing recurrence risks.
Diagnostic Imaging Techniques in Identifying Referred Pain
Cutting-edge scans provide clarity where conventional methods fall short in symptom analysis. Modern imaging technologies detect subtle tissue changes that standard examinations often miss. These tools help clinicians connect symptoms to their true origins, particularly when nerve roots or soft tissues contribute to complex cases.

The Role of CT, MR, and Dynamic MRI Protocols
Advanced imaging reveals hidden sources of discomfort through detailed anatomical views. CT scans excel at identifying bone-related compression, while MR imaging visualizes soft tissue inflammation. Dynamic MRI protocols capture joint mechanics during movement, uncovering issues static scans miss.
A 2023 study showed dynamic MRI improves diagnostic sensitivity by 28% for spinal-related symptoms. These scans detect early-stage nerve root compression before permanent damage occurs. Clinicians use these findings to create targeted treatment plans.
Provocative Testing and Local Block Procedures
Diagnostic injections temporarily numb specific areas to confirm symptom sources. When combined with imaging results, these blocks pinpoint exact compression points. Research indicates this approach increases diagnostic accuracy by 34% compared to imaging alone.
Provocative tests reproduce symptoms through controlled movements. For example, resisted shoulder rotations might reveal hidden lumbar spine issues. These methods help differentiate between overlapping conditions, ensuring therapies address primary causes rather than secondary effects.
Conservative and Interventional Treatment Strategies
Effective management of complex physical symptoms requires a strategic combination of approaches. Modern protocols prioritize non-invasive methods while reserving advanced procedures for persistent cases. This balanced framework helps active individuals regain function without unnecessary risks.

Pharmacotherapy and Physical Therapy Approaches
First-line treatment often combines anti-inflammatory medications with structured exercise programs. A 2023 Canadian study found 68% of patients improved significantly using this dual approach. Therapists apply manual techniques like trigger point therapy to release muscle tension and restore mobility.
“Targeted exercise regimens correct movement imbalances that perpetuate discomfort – they’re the foundation of sustainable recovery.”
Dry needling has emerged as a key intervention for stubborn muscle knots. This technique involves inserting fine needles into hyperirritable tissue, disrupting pain signals. Clinical trials show it enhances traditional therapy outcomes by 22% when used appropriately.
Interventional Techniques: Injections and Radiofrequency Treatments
When conservative methods plateau, injections offer targeted relief. Corticosteroid formulations reduce inflammation near joints or nerves, while platelet-rich plasma (PRP) promotes healing. Recent guidelines recommend these interventions for symptoms lasting beyond 6 weeks.
| Technique | Application | Success Rate | Recovery Time |
|---|---|---|---|
| Trigger Point Injections | Muscle knots | 74% | 2-4 days |
| Radiofrequency Ablation | Chronic joint issues | 82% | 1-2 weeks |
| Prolotherapy | Ligament laxity | 68% | 3-5 days |
Radiofrequency treatments use heat to disable problematic nerves temporarily. A 2022 multicenter study demonstrated 8-month relief durations in 79% of cases. These methods prove particularly effective for athletes needing rapid return to training.
Role of Physical Therapy and Trigger Point Interventions
Targeted therapy approaches break persistent discomfort cycles in active bodies. Specialized techniques address both surface symptoms and underlying causes, offering relief where general treatments fall short. Modern protocols combine hands-on methods with advanced interventions for comprehensive care.
Revolutionary Approaches in Muscle Recovery
Dry needling and trigger point injections disrupt dysfunctional tissue patterns effectively. A 2023 study in the Journal of Manual Therapy showed these methods reduce muscle tightness by 58% within three sessions. Patients report improved mobility and decreased localized symptoms after treatment.
“Precision interventions reset neuromuscular communication pathways, creating lasting changes in tissue behavior.”
| Technique | Mechanism | Effect Duration | Success Rate |
|---|---|---|---|
| Dry Needling | Deactivates trigger points | 4-7 days | 79% |
| Trigger Point Injections | Reduces inflammation | 2-3 weeks | 82% |
| Myofascial Release | Improves tissue mobility | 5-10 days | 68% |
Clinical practice reveals most patients need 4-6 sessions for sustained improvement. Therapists customize protocols based on symptom patterns and activity demands. This personalized approach prevents recurrence by addressing individual movement imbalances.
Calgary-based clinics report 73% faster recovery times when combining these methods with corrective exercises. Ongoing assessments ensure treatments adapt as tissue responses evolve, maintaining progress toward long-term goals.
Integrative Rehabilitation and Return-to-Play Protocols
Tailored rehabilitation programs bridge the gap between injury recovery and peak performance. These protocols address both physical limitations and neural adaptations that hinder optimal movement. Modern approaches combine corrective exercises with neuromuscular retraining to rebuild strength while preventing re-injury.

Custom Exercise Programs for Recovery
Personalized regimens target specific tissue weaknesses and movement imbalances. A 2023 Canadian study revealed athletes using customized plans regained full function 23% faster than those following generic protocols. Therapists design these programs using data from:
- Biomechanical movement assessments
- Muscle activation pattern analysis
- Sport-specific demand evaluations
“Programs blending strength training with proprioceptive drills reduce re-injury rates by 41% in contact sports.”
| Rehabilitation Phase | Focus Areas | Key Exercises | Success Rate |
|---|---|---|---|
| Acute Recovery | Inflammation control | Isometric holds | 89% |
| Strength Building | Muscle activation | Eccentric loading | 78% |
| Return-to-Play | Sport-specific drills | Plyometrics | 92% |
Continuous monitoring ensures exercises adapt to each patient’s progress. Therapists track range-of-motion improvements and functional capacity weekly. This dynamic approach addresses emerging weaknesses before they trigger new issues.
Patients completing integrated programs show 67% better long-term outcomes in affected areas compared to standard treatments. Regular reassessments maintain alignment between therapeutic goals and the patient’s recovery trajectory, creating sustainable results for active Canadians.
Research Insights: Studies on Pain Referral Patterns
Recent advancements in sports medicine research have reshaped how professionals approach complex symptom patterns. Investigations into bodily signal misinterpretation reveal critical insights for clinical practice.
Review of Key Research and Epidemiology Studies
A 2021 Canadian study tracked 1,200 athletes over three seasons. Findings showed 34% experienced discomfort unrelated to injury sites during their careers. Researchers identified shoulder-to-elbow and hip-to-knee patterns as most prevalent.
“Multi-center trials demonstrate 68% accuracy improvement when combining movement analysis with patient history reviews.”
Epidemiology data highlights specific risk factors:
- Overhead sports participants show 2.3x higher incidence rates
- Endurance athletes report 41% more lumbar-related thigh sensations
- Contact sport professionals experience quicker symptom migration
| Study Focus | Sample Size | Key Finding |
|---|---|---|
| Neural Pathways | 450 cases | 62% involved cross-nerve signaling |
| Rehabilitation Outcomes | 890 patients | Early intervention cut chronic cases by 57% |
| Diagnostic Accuracy | 1,040 assessments | Combined methods improved detection by 73% |
Methodologically rigorous investigations employ motion capture technology and pressure mapping. These tools help correlate movement abnormalities with reported symptom locations. Current protocols now integrate these findings into standardized evaluation frameworks.
Ongoing research continues refining treatment approaches. Updated guidelines emphasize personalized care plans based on each athlete’s unique biomechanical profile and sport demands.
Effective Assessment of Pain Referral Patterns in Athletes
Accurate identification of symptom origins demands meticulous evaluation strategies. Clinicians employ structured protocols combining objective measures with patient-reported details. This dual approach helps differentiate between overlapping conditions affecting performance.
Integrating Observation With Historical Data
Modern assessment frameworks prioritize three core elements:
- Movement pattern analysis during sport-specific actions
- Detailed timeline of symptom development and triggers
- Comparative analysis of affected vs unaffected regions
“Comprehensive evaluations reduce diagnostic errors by 58% in cases involving complex symptom patterns.”
Clinicians analyze subtle variations in quality and location through targeted questioning. A runner describing calf tightness during uphill segments might reveal hidden lumbar spine dysfunction. These insights guide subsequent physical examinations.
| Assessment Component | Purpose | Clinical Tool |
|---|---|---|
| Tissue Mobility Testing | Identify restricted areas | Joint play assessment |
| Neurological Screening | Rule out nerve involvement | Reflex hammer |
| Functional Capacity | Measure performance limits | Single-leg squat test |
This systematic process enables therapists to create targeted management plans. Regular reassessments ensure treatment strategies adapt as tissue responses evolve.
Clinical Application and Practical Case Studies
Real-world examples clarify complex therapeutic challenges faced by active individuals. At Riverside Sports Therapy, our team resolves puzzling symptoms through systematic evaluation and tailored interventions. Three representative cases demonstrate how strategic approaches restore function.
Lessons From Hockey Player’s Neck-to-Shoulder Recovery
A professional hockey player reported persistent shoulder stiffness despite normal joint imaging. Assessment revealed restricted cervical rotation and latent trigger points in the trapezius. Treatment combined:
- Manual release of neck musculature
- Dry needling for trigger point deactivation
- Rotator cuff coordination drills
Symptoms resolved within 12 sessions, allowing full return to play. This case highlights how cervical dysfunction can mimic shoulder pathology.
| Technique | Application | Outcome |
|---|---|---|
| Trigger Point Dry Needling | Upper trapezius | 78% stiffness reduction |
| Joint Mobilization | C3-C5 vertebrae | Restored 92% neck rotation |
| Scapular Stabilization | Dynamic exercises | Improved throwing accuracy |
Calgary Runner’s Calf Mystery Solved
A marathoner presented with recurrent calf tightness despite stretching. Evaluation uncovered limited hip extension and lumbar facet joint irritation. Pain caused by spinal stiffness projected down the leg through shared neural pathways. Six sessions addressing core stability and spinal mobility eliminated symptoms.
“Addressing the primary source transformed this athlete’s recovery trajectory – we achieved what localized treatments couldn’t.”
Actionable Management Strategies
Effective protocols require:
- Comprehensive movement chain analysis
- Differentiation between local/referred sources
- Trigger point interventions when indicated
Weekly progress tracking ensures adaptations match tissue response patterns. Calgary-based athletes benefit from these evidence-informed approaches tailored to sport-specific demands.
Expert Strategies to Manage Athlete Pain Referral Patterns
Understanding complex bodily signals remains crucial for effective sports care. Differentiating between referred and radicular discomfort requires expertise, as symptoms often originate far from their primary source. Clinicians must combine manual evaluations with advanced imaging to uncover hidden issues driving persistent sensations.
Successful management hinges on three pillars: thorough clinical assessment, targeted treatment strategies, and ongoing research collaboration. Recent studies highlight how spinal joint dysfunction frequently mimics nerve-related issues, emphasizing the need for precise diagnostic protocols.
At Riverside Sports Therapy, our Calgary team blends evidence-based methods with individualized care plans. This approach addresses root causes rather than surface symptoms, helping active Canadians achieve lasting recovery. Our protocols integrate movement analysis, tissue-specific interventions, and progressive rehabilitation exercises.
Continued advancements in sports medicine will further refine diagnostic accuracy and therapeutic outcomes. For those experiencing puzzling physical sensations, early expert evaluation prevents chronic complications. Contact Riverside Sports Therapy at (403) 283-7551 to explore personalized solutions for your unique needs.
